
My Functional Smile
Myofunctional Therapy
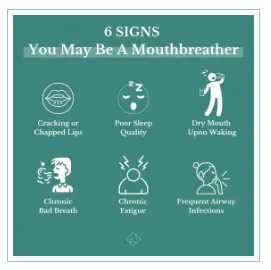
Symptoms
Facial Growth & Appearance

Breathing through the mouth can significantly impact facial structure and appearance, particularly in children who are still in their developmental stages. If left uncorrected, mouth breathing in children can lead to abnormal facial and dental growth. Common signs include elongated, narrow faces, less prominent cheekbones, smaller lower jaws, and weaker chins. Additional facial characteristics may include gummy smiles, misaligned teeth, and a "mouth breather" look, which is often perceived as less appealing.
Wider Effects on the Body
Mouth breathing interferes with the body’s natural mechanics, often stemming from insufficient oxygen intake. This disruption can trigger various issues, including:
• Headaches
• Gum disease and gingivitis
• Persistent sore throats and cold-like symptoms
• Bad breath
• Increased cavity risk
• Poor sleep quality, fatigue, and sleep apnea
• Elevated blood pressure and heart concerns
• Postural imbalances and spinal problems
• Digestive issues, such as bloating, stomach upset, and acid reflux
Specific Concerns in Children
For children, mouth breathing can have additional consequences, such as:
• Stunted growth
• Difficulty performing well academically
• Symptoms resembling ADD or ADHD
Addressing mouth breathing early is essential to prevent these physical and developmental issues.
Jaw Pain, Facial Pain and TMJ

Jaw pain, commonly referred to as temporomandibular joint dysfunction (TMD), can result from a variety of factors, including mouth breathing, teeth clenching or grinding, dental crowding, chewing on one side of the mouth, nail biting, or poor postural habits like resting the chin on a hand. TMD is often accompanied by symptoms such as headaches, neck pain, and tension in the shoulders. The tongue plays a critical role in stabilizing the jaw, and when it is not positioned or functioning correctly, the jaw joint may struggle to maintain proper stability.
Myofunctional therapy offers a non-invasive solution for managing jaw pain. By addressing muscle imbalances and tongue dysfunction, patients often experience relief from jaw discomfort and associated symptoms like headaches. Treatment approaches vary based on individual needs, and myofunctional therapists often collaborate with specialists such as orthodontists, dentists, and physical therapists. Together, they work to retrain and rebalance the muscles of the face, mouth, and neck to restore proper function.
How Myofunctional Therapy Helps with Facial Trauma, Paralysis, or Special Needs
Individuals who have experienced facial trauma, paralysis, or have special needs such as Down syndrome, cerebral palsy, or chronic pain benefit greatly from a team-based care approach. An advanced myofunctional therapist can play a vital role in this team by improving essential functions like swallowing, breathing, speech, and chewing.
By rebalancing the facial muscles, myofunctional therapy can help relieve pain, reduce swelling, enhance chewing and speech abilities, and even improve the appearance of scars. This holistic approach supports better overall function and quality of life for those facing unique challenges.
Mouth Breathing
What Is Mouth Breathing?
The primary function of the mouth is for eating, chewing, speaking, and communication, while the nose is specifically designed for breathing. However, when nasal airflow is restricted, the body compensates by breathing through the mouth. Over time, this can become a habitual practice, leading to various health issues if not corrected. Mouth breathing and keeping the mouth open are closely linked and equally harmful to long-term health.
What Causes Mouth Breathing?
Several factors can contribute to mouth breathing, including:
• Allergies or food sensitivities
• Enlarged tonsils or adenoids
• Chronic nasal congestion
• Respiratory infections
• Asthma
• Deviated septum
• Nasal polyps
The Importance of Nasal Breathing
The body is designed for nasal breathing, which offers numerous benefits:
• Filters and purifies the air, removing dust mites within 15 minutes.
• Regulates oxygen intake and supports proper tongue posture by encouraging it to rest on the roof of the mouth.
• Reduces allergy symptoms and the frequency of colds.
In contrast, mouth breathing can lead to over-breathing, disrupting the balance between oxygen and carbon dioxide, a condition known as hyperventilation. This imbalance can negatively affect bodily functions, contributing to various health problems.
How Myofunctional Therapy Can Help
For those accustomed to mouth breathing, transitioning to nasal breathing can be challenging. Over time, the muscles around the face and mouth adapt to this dysfunctional pattern, making it difficult to relearn natural breathing. Myofunctional therapy helps retrain these muscles and establish nasal breathing habits. Working with a myofunctional therapist can lead to remarkable improvements in health and overall quality of life.
Sleep Apnea

Sleep Disordered Breathing
The connection between sleep and overall health has become increasingly evident as research highlights the critical role of quality sleep in leading a happy, healthy life. While we often attribute poor sleep to modern factors like busy schedules, excessive screen time, and prioritizing work over rest, there may be deeper, underlying causes.
In some cases, sleep problems stem from physical conditions rather than lifestyle habits. One such condition is sleep disordered breathing, a group of breathing-related issues that disrupt restful sleep and can significantly impact health. While sleep apnea is widely recognized as a serious health risk, it’s not the only concern. Sleep disordered breathing encompasses a range of symptoms, from excessive snoring and teeth grinding to more severe conditions like obstructive sleep apnea.
Recognizing and addressing these issues is essential for achieving restorative sleep and protecting long-term health.
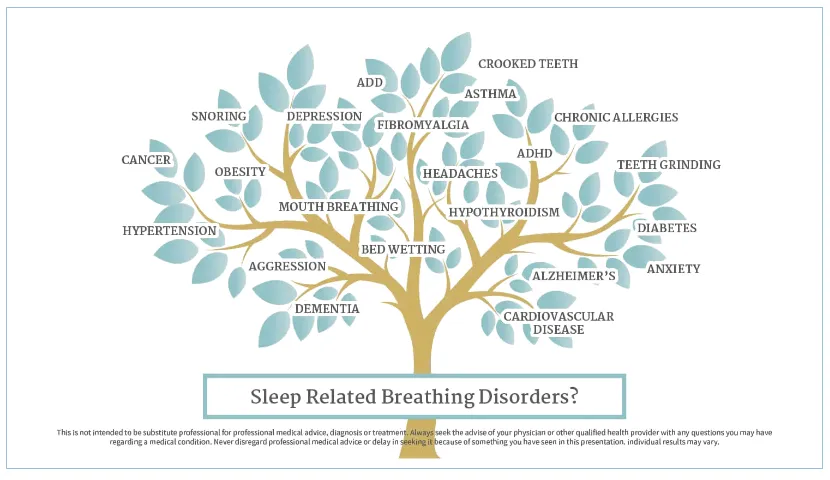
How Serious Is Sleep Disordered Breathing
Chronic sleep disordered breathing can disrupt sleep patterns night after night, leading to significant physical and mental consequences. Imagine how you feel after just a few poor nights of sleep—grumpy, fatigued, unfocused, or even nodding off during the day. Now, consider experiencing this exhaustion for months or years.
The effects of sleep deprivation go beyond feeling tired; it can contribute to serious health problems. In children, sleep apnea has been linked to developmental concerns such as ADD, lower IQ, stunted growth, and delayed physical development. For adults, chronic sleep deprivation is associated with an increased risk of long-term health conditions like heart disease, high blood pressure, and diabetes—factors that can lead to a shorter, less fulfilling life.
Does Mouth Breathing Affect Facial Development?
Mouth breathing and airway health are closely tied to sleep apnea, with a narrow airway being a major risk factor for obstructive sleep apnea. For children, habitual mouth breathing—whether caused by congestion, allergies, or tongue-tie—can significantly impact orofacial growth. This often results in narrow palates, smaller jaws, and reduced forward facial growth, leading to longer and narrower facial structures over time. Addressing mouth breathing early is crucial to preventing these developmental changes and supporting healthy growth.
Speech Problems

Myofunctional Therapy vs. Speech Therapy
While myofunctional therapy and speech therapy may address overlapping concerns, they are distinct practices. Just as dental hygienists are not trained in myofunctional therapy during their education, speech pathologists also do not receive formal training in this area.
Myofunctional therapy, however, can serve as a foundational treatment for speech issues. When the tongue and oral muscles aren’t functioning correctly, children may have difficulty producing certain sounds. From a myofunctional perspective, it’s important to address any underlying muscle dysfunction before starting a speech therapy program.
For example, difficulties with the "S" sound are often linked to tongue thrust and mouth breathing, as lisping is a common symptom. Similarly, sounds like "T," "D," "N," and "L" require precise tongue movements and placement, which can be challenging for individuals who lack proper oral muscle control. Myofunctional therapy helps both children and adults develop the muscle coordination and tongue placement needed for clear, functional speech.
How Myofunctional Therapy Supports Speech
Myofunctional therapy is not a replacement for speech therapy but can complement it by addressing the root causes of speech difficulties. By retraining the tongue and facial muscles, this therapy creates a solid foundation for speech improvement. It focuses on improving tongue posture, movement, and control, making it easier for patients to produce sounds accurately.
Whether it’s a child learning to overcome a lisp or an adult addressing long-standing speech challenges, incorporating myofunctional therapy into the treatment plan can significantly enhance outcomes.
Tongue Thrust

Do I Have a Tongue Thrust?
A tongue thrust occurs when the tongue rests low in the mouth and pushes forward during swallowing. This condition often goes hand in hand with mouth breathing, meaning if you’re a mouth breather, you likely have a tongue thrust swallowing pattern. Ideally, the tongue should rest on the roof of the mouth and push food or drink back during swallowing, not forward. When the tongue’s position and function are incorrect, issues such as Gastroesophageal Reflux Disorder (GERD) and excessive burping due to air swallowing may arise. These are key signs that myofunctional therapy may be needed.
Understanding Tongue Thrust and Its Effects
The most significant concern with tongue thrust is the tongue’s resting position. Instead of resting on the roof of the mouth, the tongue tip often sits against or between the front teeth, with the entire tongue positioned low. This improper posture disrupts the tongue’s role as an internal support system for the upper jaw.
A tongue thrust is not just a condition—it’s a symptom that often points to larger issues with airway and breathing. It is commonly accompanied by mouth breathing and an open-mouth resting posture, reinforcing the need to address these patterns.
How to Correct a Tongue Thrust
The only way to eliminate a tongue thrust is by creating new habits through an exercise-based therapy program that retrains both the muscles and the mind. Myofunctional therapy offers customized treatment plans to address individual needs and correct tongue-related issues.
Signs You or Your Child May Have a Tongue Thrust
Here are three common indicators of a tongue thrust:
• Mouth Breathing: A clear sign of tongue thrust is an open mouth at rest, often with the tongue forward or sticking out.
• Speech Difficulties: Lisping, articulation issues, and other speech problems, such as challenges with vocal quality or speaking rate, may indicate tongue thrust.
• Sucking Habits: Thumb sucking and similar habits can lead to tongue thrust by altering the swallowing pattern. Even after the habit stops, the incorrect tongue posture often persists without intervention.
Correcting a tongue thrust involves addressing these habits and retraining the tongue and oral muscles for proper function and posture.
Tongue Tie

What Is a Tongue-Tie?
Do you snore? Experience jaw pain, migraines, or headaches? Struggle with ADD/ADHD, body tension, or difficulty pronouncing certain words? Do you breathe through your mouth or grind your teeth? If so, you might have a tongue-tie.
A tongue-tie occurs when the frenum—the small strip of tissue connecting your tongue to the floor of your mouth—is too tight or restricted. While everyone has a frenum, in some people it limits the tongue's movement, leading to a variety of issues affecting oral function, breathing, and even overall health.
Tongue-ties come in two types:
1. Anterior Tongue-Tie: Easier to spot, this type restricts the underside of the tongue visibly when lifted.
2. Posterior Tongue-Tie: More subtle and often symptom-based, this type may require a closer evaluation as it is hidden beneath the floor of the mouth.
Why Does a Tongue-Tie Matter?
The tongue plays a vital role in overall health by supporting proper oral posture and function. Ideally, the tongue should rest against the roof of the mouth, providing support for the upper jaw and guiding optimal facial development. A tongue-tie, however, prevents the tongue from reaching the palate, causing it to rest at the bottom of the mouth—a dysfunctional position.
This restricted posture can lead to:
• Crooked teeth and improper jaw development
• Mouth breathing, which exacerbates other health issues
• Chronic pain in the jaw, face, and head
• Increased risk of sleep apnea and airway complications
• Facial and cranial developmental concerns in children
Studies show that tongue-tied children are particularly prone to sleep apnea, airway problems, and long-term orthodontic challenges.
What Can Be Done to Address a Tongue-Tie?
The primary treatment for a tongue-tie is a frenectomy, a simple procedure to release the restricted frenum. Proper preparation and follow-up care are critical for success:
1. Pre-Procedure Exercises: These strengthen and prepare the tongue for the new range of motion.
2. Post-Procedure Follow-Up: Within 24 hours after surgery, follow-up care involves additional exercises to maintain mobility and strengthen the tongue muscles.
Without proper preparation and retraining, the tongue may reattach to its original position, often necessitating a second procedure. Myofunctional therapy is essential for retraining the tongue’s muscles, promoting correct function, and ensuring lasting results.
Tongue-Tie Symptoms in Babies
In infants, tongue-ties are often linked to breastfeeding difficulties, but the condition can sometimes go undetected if feeding appears normal. Over time, the restricted tongue movement may influence the development of the mouth, face, and skull, contributing to:
• Speech challenges
• ADD/ADHD symptoms
• Sleep apnea or disordered breathing
• Jaw and facial pain
Addressing a tongue-tie early can prevent these complications and support healthier growth and development.
My Functional Smile
Resources
Providers

© Copyright 2026. My Functional Smile. All Rights Reserved.
The information provided on this website is not intended to serve as medical advice, nor is it meant to diagnose, treat, cure, or prevent any disease, symptom, or condition. For medical advice, please consult a qualified and licensed healthcare professional. Always speak with your doctor before starting any fitness, exercise, nutrition, or weight loss program, or making any other lifestyle changes.
My Functional Smile - Myofunctional Therapy
Copyright © 2022-2025 All Rights Reserved
Contact Us
(832)299-5803
4200 Research Forest Drive, Suite 220
The Woodlands, TX 77381
The information provided on this website is not intended to serve as medical advice, nor is it meant to diagnose, treat, cure, or prevent any disease, symptom, or condition. For medical advice, please consult a qualified and licensed healthcare professional. Always speak with your doctor before starting any fitness, exercise, nutrition, or weight loss program, or making any other lifestyle changes.
My Functional Smile - Myofunctional Therapy
Copyright © 2022- 2025 All Rights Reserved