My Functional Smile
Myofunctional Therapy
Because cavities, mouth breathing, and poor sleep
usually mean something more.
We find what’s been missed—and help your child feel better, for good.
Because Cavities, Mouth Breathing, and Poor Sleep usually mean something more.
We find what’s been missed—and help your child feel better, for good.
What is Myofunctional Therapy?
Myofunctional therapy is a type of treatment aimed at addressing orofacial myofunctional disorders, which refer to improper muscle function in the mouth and face. These disorders can affect a person's ability to speak, chew, swallow, and breathe properly. Myofunctional therapy typically involves exercises to strengthen and retain the muscles involved in these functions.
To identify orofacial myofunctional disorders, a trained professional can evaluate a patient's oral and facial muscle movements, breathing patterns, and speech, as well as any associated symptoms such as mouth breathing, tongue thrusting, or snoring. We offer treatment in person and totally virtual for your convenience!!
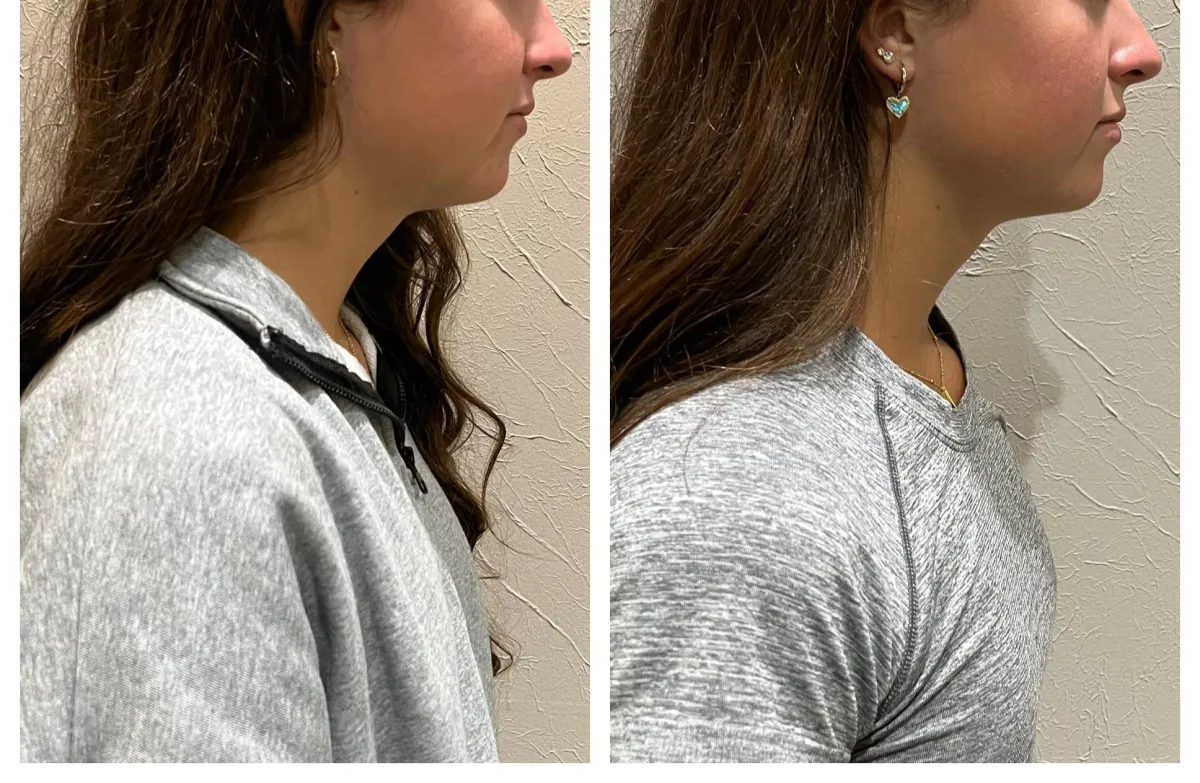
Take a look at some of our results!
What is Myofunctional Therapy?
Myofunctional therapy is a type of treatment aimed at addressing orofacial myofunctional disorders, which refer to improper muscle function in the mouth and face. These disorders can affect a person's ability to speak, chew, swallow, and breathe properly. Myofunctional therapy typically involves exercises to strengthen and retain the muscles involved in these functions.
To identify orofacial myofunctional disorders, a trained professional can evaluate a patient's oral and facial muscle movements, breathing patterns, and speech, as well as any associated symptoms such as mouth breathing, tongue thrusting, or snoring. We offer treatment in person and totally virtual for your convenience!!
Take a look at some of our results!
Who needs Myofunctional Therapy?
You may notice signs or symptoms that suggest your child could benefit from myofunctional therapy. These signs can include:
Mouth breathing
Snoring or sleep apnea
Chronic allergies or sinus problems
Difficulty chewing or swallowing
Speech difficulties
Tongue thrusting or thumb sucking
Dental malocclusions, such as an overbite or underbite
Drooling past the age of 2 years old
Chronic headaches or neck pain

Who needs Myofunctional Therapy?
You may notice signs or symptoms that suggest your child could benefit from myofunctional therapy. These signs can include:

Mouth breathing
Snoring or sleep apnea
Chronic allergies or sinus problems
Difficulty chewing or swallowing
Speech difficulties
Tongue thrusting or thumb sucking
Dental malocclusions, such as an overbite or underbite
Drooling past the age of 2 years old
Chronic headaches or neck pain
What if a few simple changes could drastically
improve your family's sleep?
Imagine...
There was a way to effortlessly wake up feeling refreshed, with anxiety and stress melting away after a full night of deep, restorative sleep...
You could finally have peaceful nights where you and your loved ones sleep soundly, waking up ready to tackle the day with energy and focus...
You could strengthen your family bonds, as everyone feels more connected and patient, thanks to the calm and clarity that come from proper rest...
You could enjoy your daily routines without the constant fatigue, sickness, or irritability that poor sleep once brought into your life..
And all of this could be achieved with a few simple changes that transform your nights, leading to happier, healthier days for everyone...
What our Clients are saying...
⭐⭐⭐⭐⭐
" Sarah is the real deal! She is the superhero of tongue exercises – friendly, fun, and downright effective. She turned my exercises into a playful challenge, and I'm thrilled with the results! The sessions were a blast, and her enthusiasm made the whole journey a joyride. If you're thinking about Myofunctional Therapy, look no further than My functional Smile. It's not just therapy; it's changing my son's life. He is sleeping better, better behaved a school and overall healthier. I can't thank her enough for helping our family. "
~ Bernalea Liesse
⭐⭐⭐⭐⭐
" Tongue Tied at 5 causing all sorts of speech, swallowing, eating and sleep issues. Sarah was our advocate that we so desperately needed to resolve these issues! Over the last several months, Sarah has worked diligently with us to get our son's tongue tie released. She went above and beyond with guiding, educating, and following up with us on all of the tongue tie exercises and post procedure. We were so impressed on how she worked so well with a hyper 5 year old, keeping him focused on the task at hand. She worked cohesively with Dr. Jessica Kacher and her team during the tongue tie procedure (God Bless the patience of Pediatric Dentists!) We are going to be forever grateful for Sarah and the team."
~ Christie Turner
⭐⭐⭐⭐⭐
" I had an exceptional experience with Sarah at My Functional Smile. Her expertise and personalized approach were evident from the start. She is attentive, knowledgeable, and made the sessions enjoyable. Sarah's genuine care for my son’s progress and ability to work with my 7 year old truly stood out. She is incredibly gifted when it comes to working with kids of any age. I highly recommend Sarah and her work to anyone seeking top-notch care in myofunctional therapy."
~ Lauren Weber
The Multidisciplinary Approach
A multidisciplinary approach to myofunctional therapy is essential for its success because orofacial myofunctional disorders are often complex and can have multiple underlying causes. By involving various healthcare professionals such as dentists, speech therapists, ENTs, chiropractors, and orthodontists, a comprehensive evaluation and treatment plan can be created.
The interdisciplinary team can work together to address all aspects of the disorder, including dental issues, breathing problems, speech difficulties, and more. This approach ensures that the patient receives the most effective and individualized treatment possible, leading to better outcomes and
improved quality of life.
Frequently Asked Questions
What is the right age for myofunctional therapy?
The truth is, it's rarely too early, and it's certainly not too late to address oral myofunctional disorders.
For Younger Children (Ages 4-6): This age range is often ideal because a child's muscles and bones are still very pliable and developing. Early intervention can gently guide proper growth and establish healthy habits before compensatory patterns become deeply ingrained. At this age, therapy is typically introduced through fun, engaging activities and games.
For School-Aged Children and Teens (Ages 7-18): Significant progress can still be made. While some habits may be more established, children and adolescents are often highly motivated and capable of learning new neuromuscular patterns. Addressing these issues can support ongoing orthodontic treatment, improve sleep quality, and enhance overall well-being.
Ultimately, if you have concerns about your child's breathing, oral posture, or dental development, it's always a good time to consider an evaluation.
How does myofunctional therapy work?
Myofunctional therapy works like a targeted training program for the muscles of the mouth and face. We begin with a thorough assessment to identify any dysfunctional patterns in your child's breathing, swallowing, and resting oral posture. Based on this assessment, I design a personalized program of gentle, yet effective, exercises. These exercises are practiced for short durations daily, helping to retrain the neuromuscular patterns. The goal is to build muscle memory and establish new, healthy habits, leading to improved function and long-term stability.
What benefits will my child see?
The benefits of myofunctional therapy often extend far beyond just the mouth. Parents frequently report a wide range of positive changes in their children:
Improved Nasal Breathing: Learning to breathe through the nose consistently is critical for overall health, leading to better oxygen intake and filtration.
Enhanced Sleep Quality: Proper breathing patterns can significantly reduce issues like snoring, teeth grinding, and restless sleep, resulting in more restorative sleep. This often translates to improved energy, focus, and behavior during the day.
Support for Dental Development: Correct tongue posture and lip seal provide natural forces that help guide the development of the jaws and teeth, often leading to more stable orthodontic outcomes.
Clearer Speech: Strengthening oral muscles can improve articulation and reduce speech impediments related to tongue placement.
Better Chewing and Swallowing: Efficient chewing and swallowing contribute to better digestion and can help address picky eating habits.
Overall Health and Well-being: When foundational functions like breathing and sleep improve, children often experience increased vitality, better concentration at school, and improved mood.
These benefits contribute to a child's holistic development, fostering healthier habits that can impact their physical and cognitive well-being.
What signs indicate a tongue-tie?
People with a tongue-tie often breathe through their mouth, which can result in a variety of myofunctional problems and symptoms. Common issues include chronic jaw pain, sleep apnea, facial pain, headaches, and teeth clenching or grinding, as well as dental and orthodontic concerns. Studies indicate that tongue-tied children have a higher risk of developing sleep apnea and airway problems, and their facial and cranial growth can also be affected.
What is the purpose of a tongue tie release?
A tongue tie, or ankyloglossia, occurs when the tissue under the tongue (frenum) restricts its normal movement. The primary purpose of a tongue tie release (frenectomy) is to free the tongue, allowing it to achieve its full range of motion and function properly. This improved mobility is critical for effective eating, for children to develop clear speech, and for individuals of all ages to maintain healthy oral posture, encourage proper nasal breathing, and support optimal jaw and facial development.
Tongue tie releases are most effective when they are done in conjunction with myofunctional therapy to ensure the newly freed tongue learns to use its enhanced mobility effectively, optimizing long-term benefits for oral health and overall well-being.
My kid grinds their teeth. Is this normal?
Teeth clenching or grinding can indicate an airway problem. When you stop breathing during sleep, your brain sends a signal to your mouth to clench or grind in an effort to keep the mouth open. This is often a sign of a tongue-tie, where the tongue rests too low in the mouth, falling back into the airway and blocking the flow of oxygen.
Which specialists should I consult for jaw pain?
Because temporomandibular disorders (TMD) are complex, effectively managing and treating TMJ pain and related symptoms often requires a skilled, multi-disciplinary approach. A knowledgeable myofunctional therapist can play a key role in helping patients connect with the right doctors and specialists for TMD care. As a myofunctional therapist, part of my role is to guide patients to the specific healthcare professionals they need for their treatment team.
Over the years, we have developed a strong referral network, which enables us to recommend the most suitable doctor, dentist, or orthodontist based on the individual needs of my patients dealing with TMJ-related concerns.
This is a lot of money... Is it worth it?
Absolutely, yes. Myofunctional therapy is an investment in your child's long-term health and development. The therapy addresses foundational issues related to breathing, swallowing, and oral posture that can have widespread effects. By correcting these patterns early, you can help mitigate the need for more extensive interventions later, such as repeated orthodontic treatment, and potentially reduce the risk of future health issues like sleep-disordered breathing. The skills learned in therapy are lifelong, promoting healthier habits that support overall well-being for years to come.
Is insurance accepted at your practice?
We understand that healthcare costs can accumulate, but My Functional Smile is an out-of-network provider and cannot bill insurance.
Choosing to work with an out-of-network provider offers greater transparency in treatment costs for both the patient and the provider. This allows us to focus on your needs instead of working under the constraints of insurance companies. Our pricing is clear from the start, with no hidden fees, co-pays, or premiums. At My Functional Smile, we prioritize working directly for our patients, not for insurance companies that control the time spent with you and what treatments are prioritized.
Additionally, we accept FSA and HSA payments and provide the necessary receipts.
My Functional Smile
Resources
Providers

© Copyright 2025. My Functional Smile. All Rights Reserved.
The information provided on this website is not intended to serve as medical advice, nor is it meant to diagnose, treat, cure, or prevent any disease, symptom, or condition. For medical advice, please consult a qualified and licensed healthcare professional. Always speak with your doctor before starting any fitness, exercise, nutrition, or weight loss program, or making any other lifestyle changes.
My Functional Smile - Myofunctional Therapy
Copyright © 2022-2025 All Rights Reserved
Contact Us
(832)299-5803
4200 Research Forest Drive, Suite 220
The Woodlands, TX 77381
The information provided on this website is not intended to serve as medical advice, nor is it meant to diagnose, treat, cure, or prevent any disease, symptom, or condition. For medical advice, please consult a qualified and licensed healthcare professional. Always speak with your doctor before starting any fitness, exercise, nutrition, or weight loss program, or making any other lifestyle changes.
My Functional Smile - Myofunctional Therapy
Copyright © 2022- 2025 All Rights Reserved